Lots of people talk about the thyroid, but do we really understand what it does, what symptoms indicate it’s not functioning optimally, and how to support it naturally through diet, lifestyle, and targeted supplement strategies? Let’s take a look at this amazing gland and how we can best take care of it.
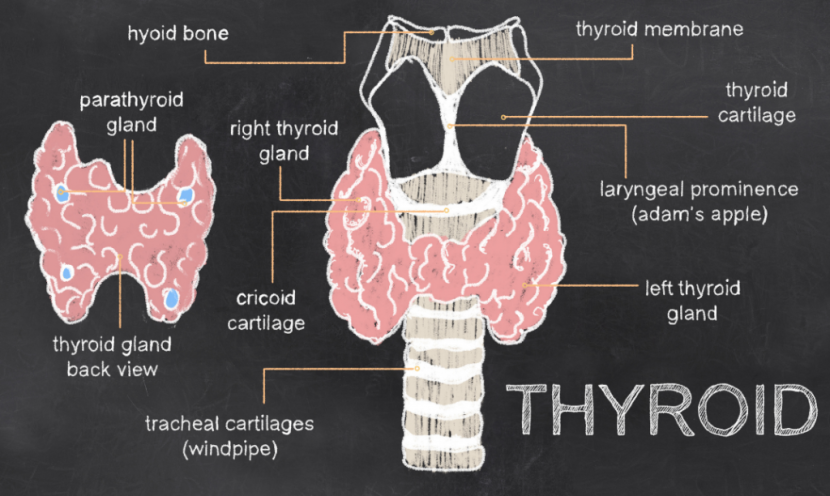
The thyroid is a small, butterfly-shaped organ that sits in the front of the neck. It has two lobes, or halves, that sit alongside the trachea (the windpipe), joined by a small band of thyroid tissue known as the isthmus.
What does the thyroid actually DO?
The impact of your thyroid is vast: it influences almost every single cell in your body!
When we think of the thyroid, most people first think of metabolism. Indeed, regulating our metabolism is one of the thyroid’s primary roles in governing how the body uses energy, consumes oxygen, and produces heat. But the thyroid is critical to our health in so many different ways:
- It controls our Basal Metabolic Rate (BMR) which is the measurement of the amount of oxygen used by the body when at rest (Mullur 2014 ).
- It controls our body temperature by influencing heat production (Filfilan 2023).
- It’s also important for the metabolism of our macronutrients: it influences glucose metabolism and controls the use of fat for energy (Eom 2022 ). This is one reason people with sluggish thyroid function may gain weight and can’t shed it: their thyroid controls the rate at which the body uses fat as a source of fuel.
- Thyroid hormones are critical for our neurological health, particularly during fetal development (Bernal 2000 ). If the mother or child is hypothyroid, this can have severe and long-lasting effects on the neurological development of the fetus. (Levie 2019)
- For kids, the thyroid controls their growth rate (Al-Oman 2023). For adults, it influences our mental functioning and ability to focus. Many people with hypothyroidism say they feel really mentally sluggish. (Lekurwale 2023) This may be one reason why.
- Our thyroid influences our cardiovascular health as well, influencing heart rate and the amount of blood pumped by the heart (Vargas-Uricoechea 2014). It also has an indirect effect on the cardiovascular system by its influence on lipid metabolism – thyroid hormones regulate how the body synthesizes, mobilizes, and degrades cholesterol and a sluggish thyroid can lead to a buildup of cholesterol in the blood (Jonklaas 2024 ). Oftentimes we see elevated lipids on a blood chemistry panel when someone is hypothyroid.
- The thyroid affects our muscles, influencing function. When thyroid hormones are low, muscles may cramp and be painful to touch. (Fariduddin 2024 ) .
- Thyroid hormones affect our bone health and have a role in both breaking down and building bone (a process called bone remodeling) (Ladermann 2020 ).
- Our thyroid also has a strong influence on the digestive process, in particular regulating our digestive motility. One of the most common symptoms of an under-functioning thyroid is constipation and sluggish digestion. (Xu 2024 )
- The thyroid also influences our reproductive hormones, influencing both estrogen and testosterone production (Kjaergaard 2021 ). For females, low thyroid hormone output can inhibit ovulation, having a dramatic effect on one’s fertility. Hypothyroidism is also associated with a higher incidence of miscarriage. (Koyyada 2020) One of the key blocking factors for those struggling to conceive is poor thyroid function.
- And lastly, thyroid hormones support healthy skin and hair by promoting sufficient hydration and cell turnover. One of the symptoms of hypothyroidism is dry skin and thinning hair. A classic sign of hypothyroidism is the loss of the lateral 3rd of the eyebrow (this is something you’ll recognize immediately if you have it). (Santos Silva 2020; Hussein 2023)
So, yeah… the thyroid. It’s about a lot more than just metabolism!
What are the signs and symptoms that something is awry with my thyroid?
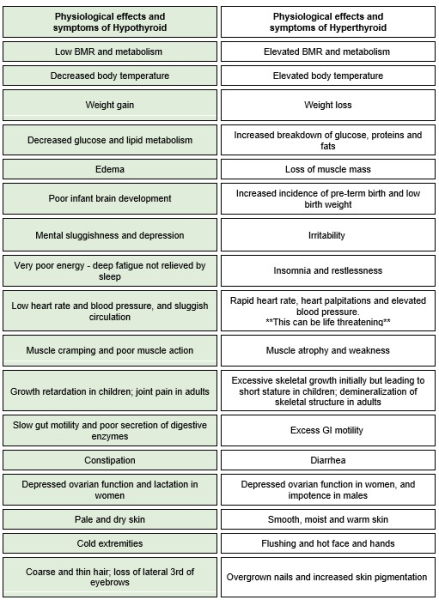
Now that we’ve learned that the thyroid plays a role in so much more than just our metabolism, many of the signs and symptoms will make more sense. We talk most often about a sluggish thyroid, known as hypothyroidism because it’s much more common than a hyper-functioning thyroid. However, an overactive thyroid can be just as problematic and in some ways more dangerous than one that’s under-functioning.
Here’s a table that shows the different symptom presentations for both types of dysfunction:
What is my bloodwork telling me?
As Restorative Wellness Practitioners, we spend a lot of time helping our clients understand the various hormones and markers included on a blood test that’s assessing thyroid function. It’s important to know what these numbers mean so you can understand what is happening in your body when you get your test results.
The two primary markers included on most conventional panels are TSH and Free T4, but this is just a small piece of the puzzle. Let’s go through a much more complete set of markers and understand how they all fit together. (Sidenote: you can always ask your doctor to run this full list of markers rather than just the TSH and Free T4!)
TSH – Thyroid Stimulating Hormone – is actually a pituitary hormone. The pituitary acts like a project manager, telling your thyroid what to do: increase thyroid hormone production or slow it down. This marker is counterintuitive: when it’s elevated, it’s indicating reduced thyroid function and when it’s low, it’s indicating elevated thyroid function. Think of it this way: when TSH is elevated, this is akin to your pituitary yelling at the thyroid – the pituitary is not getting the response it wants, so it’s raising its voice (I’m sure all parents reading this can relate ;). When TSH is low, the pituitary is just whispering to the thyroid because there’s so much thyroid hormone circulating, and it doesn’t need much. Make sense?
Now we get into the thyroid hormones themselves. There are two primary thyroid hormones released by the thyroid: T4 (thyroxine) and T3 (triiodothyronine). T4 is the inactive form, meaning it doesn’t impact your cells while T3 is the active form. The thyroid makes more T4 than T3 so the body has developed ways to transform T4 (the precursor or raw materials) into T3 (the finished product). As the active form of the hormone, T3 is one of the most important indicators of thyroid function and determines how you actually feel in your body.
When it comes to your blood panel, there are two forms of both T4 and T3: Total and Free. Total T4 or T3 is the hormone bound to a protein-carrier (think of this like a shuttle escorting the hormone through your system); Free T4 or T3 is not bound to that protein, meaning it’s available to be used by the body in whatever way is needed. And so we have the following markers on a more complete thyroid panel:
- Total T4 – the total, protein-bound form of the precursor thyroid hormone T4
- Free T4 – the free, unbound form of the precursor thyroid hormone T4 (this is a small fraction of total T4)
- Total T3 – the total, protein-bound form of the active thyroid hormone T3
- Free T3 – the free, unbound form of the active thyroid hormone T3 – this is an incredibly important hormone to assess as it’s what will directly impact how you feel
You may also see a marker called rT3 or reverse T3 on your panel – this is the metabolically inactive form of T3. The liver converts a percentage of T4 into rT3 to maintain homeostasis in the body.
Lastly, there are two antibodies that we always like to include on our thyroid panels: TPO Antibodies and Tg Antibodies.
TPO Antibodies are antibodies to thyroid peroxidase (TPO), the enzyme responsible for producing thyroid hormones. When we see elevated antibodies to this enzyme, it tells us the immune system is flagging this enzyme for attack – an indicator of an autoimmune response to the thyroid.
Tg Antibodies are antibodies to thyroglobulin (TGB), which is a protein produced by the thyroid that stores thyroid hormone (Di Jeso 2016). When we see elevated antibodies to this thyroid storage protein, it may be another indicator of thyroid autoimmunity though it can be found in other conditions as well (Kwanhoon 2020 ).
As you can see, there is so much more to the story than just TSH and Free T4! When we’re evaluating thyroid markers, we want to see if this is a basic case of thyroid dysfunction, or is it an issue with the conversion of T4 to T3? Is it an over-conversion of T4 to the metabolically inactive rT3? Is it an autoimmune situation, in which case the root cause is immune in origin rather than a malfunction of the thyroid itself? There are so many different possibilities and the only way to assess them properly is to have a complete picture of the thyroid hormones in all their different forms.
How do I care for my thyroid naturally?
When it comes to thyroid function, there are certain things that are absolutely essential for bringing it back into balance regardless of your symptom presentation or thyroid hormone labs.
Say good-bye to gluten
Here’s the thing: gluten is a big deal for most health issues, but it’s a major deal for the thyroid, particularly autoimmune thyroid conditions like Hashimoto’s, which accounts for the vast majority of low-functioning thyroid presentations (Patil 2024 ).
There are many reasons for this, but the one we want to highlight is a mechanism called “molecular mimicry”. At a molecular level, gluten proteins and thyroid tissue look almost identical – their peptide chains are extremely similar. If there is any kind of immune response to gluten (this extends far beyond Celiac Disease to any kind of sensitivity), the immune system can get confused and attack not only the gluten but also the thyroid. This is a key consideration in the development of autoimmunity.
Get a handle on your stress
There is a strong relationship between your thyroid and your adrenal glands, which are your body’s primary stress-handling glands. While this is more complex than we have the time to go into here, chronic stress will impact the communication channels between the various endocrine glands (the hypothalamus, pituitary, adrenals, thyroid, and reproductive organs) and will impact the body’s ability to convert the precursor T4 into the active thyroid hormone T3, while also making cells less receptive to thyroid hormones overall – meaning they aren’t as effective at doing their jobs throughout the body.
Ensure you are getting enough of these nutrients
There are several core nutrients that are essential for the production of thyroid hormones, the conversion of T4 to T3, and the sensitivity of cells to thyroid hormones:
- The minerals zinc, selenium, magnesium and iodine are all critically important nutrients for the production of thyroid hormones and all of these are common deficiencies. (Soares Severo 2019; Barchielli 2022; Zhou 2022; Sorrenti 2021) However, before adding selenium and iodine to your supplement regime, it is highly recommended that you work with a skilled practitioner who can determine the need for supplementation as well as the appropriate dose.
- –*Important note: for those with thyroid autoimmunity, iodine supplementation can cause a flare, and so we recommend assessing thyroid antibodies before supplementing with this nutrient. You can still consume food sources of iodine such as seafood and seaweed.
- Vitamins A, B2, B3, B6, C and D are other key nutrients to support thyroid health (Ma 2022; Bajaj 2016; Appunni 2021)
Balance your blood sugar levels
Imbalanced blood sugar has a profound impact on all aspects of the endocrine system (of which the thyroid is a part) and in addition to eliminating gluten from the diet, this is one of the most important dietary strategies you can adopt.
Heal your gut
We already talked about how impaired thyroid function can affect the digestive process, but it works both ways: impaired digestion will negatively affect your thyroid hormone production. For one, in addition to the liver, the health of the gut microbiome is another key consideration in thyroid function (Liangzhuo 2023) .
Also, an impaired gut lining is a key source of immune issues, as 80% of the immune system lives in and around the digestive tract. Since the vast majority of thyroid issues are autoimmune in origin, relieving any kind of burden on the immune system is imperative to healing.
Lastly, the nutrients required for thyroid hormone production and conversion need to be accessed from the diet, and our diet is only as good as our digestive process.
Ultimately, if you suspect or know that you have thyroid dysfunction, whetherit is hypo- or hyper-functioning and whether it is autoimmune in nature or not, your best bet is to work with a seasoned functional health practitioner who can help you pinpoint and correct the root imbalances that are driving the thyroid issues in you specifically.
If you’re a practitioner looking to learn more about how to help your clients feel better, faster, you can learn more about our comprehensive clinical training program on our curriculum page.
—-
REFERENCES
Al-Oman AF, Omer ZK. The impact of juvenile hypothyroidism on stature. J Med Life. 2023;16(8):1211-1214.
Appunni S, Rubens M, Ramamoorthy V, Saxena A, Tonse R, Veledar E, et al. Association between vitamin D deficiency and hypothyroidism: results from the National Health and Nutrition Examination Survey (NHANES) 2007-2012. BMC Endocr Disord. 2021;21(1):224.
Bajaj JK, Salwan P, Salwan S. Various possible toxicants involved in thyroid dysfunction: a review. J Clin Diagn Res. 2016;10(1):FE01-FE-03.
Barchielli G, Capperucci An, Tanini D. The role of selenium in pathologies: an updated review. Antioxidants (Basel). 2022:11(2):251.
Bernal J, Feingold KR, Anawalt B, Blackman MR, Boyce A, Chrousos G, et al. Thyroid hormones in brain development and function. In: Endotext [Internet]. South Dartmouth, MA: MDText.com, Inc; 2000. PMID 25905404.
Di Jeso B, Arvan P. Thyroglobulin from molecular and cellular biology to clinical endocrinology. Endoc Rev. 2016;37(1):2-26.
Eom YS, Wilson JR, Bernet VJ. Links between thyroid disorders and glucose homeostasis. Diabetes Metab J. 2022;46(2):239-256.
Fariduddin MM, Haq N, Bansal N. Hypothyroid myopathy. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2024. PMID 30137798.
Filfilan WM. Thyroid hormones regulate the thermoregulatory mechanisms of the body: review. Pak J Biol Sci. 2023;26(9):453-457.
Hussein RS, Atia T, Bin Dayel S. Impact of thyroid dysfunction on hair disorders. Cureus. 2023;15(8):e43266.
Jonklaas J. Hypothyroidism, lipids, and lipidomics. Endocrine. 2024;84(2):293-300.
Kjaergaard AD, Marouli E, Papadopoulou A, Deloukas P, Kus A, Sterenborg R, et al. Thyroid function, sex hormones and sexual function: a Medelian randomization study. Eur J Epidemiol. 2021;36(3):335-344.
Koyyada A, Orsu P. Role of hypothyroidism and associated pathways in pregnancy and infertility: clinical insights. Tzu Chi Med J. 2020;32(4):312-317.
Kwanhoon J, Lim D-J. Clinical implications of anti-thyroglobulin antibody measurement before surgery in thyroid cancer. Korean J Intern Med. 2018;33(6):1050-1057.
Ladermann F, Tsourdi E, Hofbauer L, Rauner M. Thyroid hormone actions and bone remodeling – the role of the Wnt signaling pathway. Exp Clin Endocrinol Diabetes. 2020;128(6-07):450-454.
Lekurwale V, Acharya S, Shukla S, Kumar S. Neuropsychiatric manifestations of thyroid diseases. Cureus. 2023;15(1):e33987.
Levie D, Korevaar TIM, Bath SC, Murcia M, Dineva M, Llop S, et al. Association of maternal iodine status with child IQ: a meta-analysis of individual participant data. J Clin Endocrinolog Metab. 2019 ;104(12) :5957-5967.
Liangzhuo X, Zhao H, Chen W. Relationship between gut microbiome and thyroid function: a two-sample Mendelian randomization study. Front Endocrinol. 2023;14:1240752.
Ma B, Yang P, Gao J, Sheng C, Usman T, Wang X, et al. Relationship of vitamin A and thyroid function in individuals with obesity and after laparoscopic sleeve gastrectomy. Front Nutr. 2022;9:824193.
Mullur R, Liu Y-Y, Brent GA. Thyroid hormone regulation of metabolism. Physiol Rev. 2014;94(2):355-382.
Patil N, Rehman A, Anastasopoulou C, Jialal I. Hypothyroidism. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2024. PMID: 3037821.
Santos Silva T, Baptista de Almeida Faro G, Bonfim Cortes MG, Pedreira de Almeida Rego VR. Primary hypothyroidism with exuberant dermatological manifestations. An Bras Dermatol. 2020;95(6):721-723.
Soares Severo J, Silva Morais JB, Coelho de Freitas TE, Pereira Andrade AL, Feitosa MM, Fontenelle LC, et al. The role of zinc in thyroid hormones metabolism. Int J Vitam Nutr Res. 2019;89(1-2):80-88.
Sorrenti S, Baldini E, Pironi D, Lauro A, D’Orazi V, Tartaglia F, et al. Iodine: Its role in thyroid hormone biosynthesis and beyond. Nutrients. 2021;13(12):4469.
Vargas-Uricoechea H, Herman Sierra-Torres C. Thyroid hormones and the heart. Horm Mol Biol Clin Invest. 2014;18(1):15-26.
Xu G-M, Hu M-X, Li S-Y, Ran X, Zhang H, Ding X-F. Thyroid disorders and gastrointestinal dysmotility: an old association. Front Physiol. 2024;15:1389113.
Zhou Q, Xue S, Zhang L, Chen G. Trace elements and the thyroid. Front Endocrinol (Lausanne). 2022;13:904889.







