Biofilm. Whether you realize it or not, you come into contact with it every single day. You know when you forget to wash out your water bottle and when you find it, the insides are a little slimy? That’s biofilm.
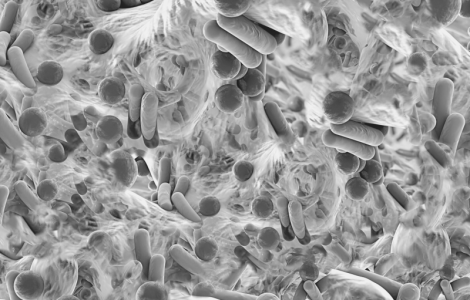
Biofilm form when bacteria adhere to surfaces in the presence of water and excrete a slimy, glue-like substance that can stick to all kinds of things – metals, plastics, your water bottle, river rocks, medical implants, and living tissue, among others. Biofilm typically consist of many species of bacteria, as well as fungi, algae, protozoa, and other debris. Essentially, a biofilm may form on any surface exposed to bacteria and water.
When it comes to health, gut health in particular, biofilm play an important role. The mucus-rich epithelial lining of the gastrointestinal tract is an ideal surface for the adhesion of free-floating microorganisms, particularly when it is damaged. The microorganisms stick to the lining of the GI tract and produce a gooey substance known as an extracellular polymeric substance (EPS), which is a network of sugars, proteins, and nucleic acids. This is the biofilm. Not only does the biofilm contain the microorganisms, this gooey mass can also sequester nutrients – especially minerals – as well as heavy metals. Over time, layers of biofilm build up, creating a bulbous, 3-dimensional “community” of microorganisms embedded and protected in this biofilm matrix.
Why do we care?
Well, all manner of pathogens use biofilm to protect themselves, in particular parasites, fungi, and pathogenic bacteria. Multiple species can and often do inhabit the same biofilm matrix, sharing nutrients and genetic material, and changing the environment around them to be more resistant to both immune cells and antimicrobials. They build up a mucous-like mass around them that can make them impervious to eradicating agents.
This means if you’ve got a client with a fungal overgrowth for example, in order to get at the fungus, we must break through the biofilm first.
When do we address it?
There are no specific symptoms that will present with biofilm, nor is there a specific GI marker for it. It’s also impossible to know if it’s present, and if present, how thick it is and what it contains. Clinically, whenever we encounter any pathogenic presence, we want to assume it is present and address it accordingly.
While there’s no direct way to test for biofilm, testing is still invaluable.
Why? Because, we only use a biofilm disruptor in a gut healing protocol when we see evidence of a pathogen that requires eradication on a stool test. And, even then we only use it on select pathogens – namely inflammatory opportunistic bacteria, fungal overgrowth, and parasites.
How do we address it?
If you suspect biofilm is part of your client’s GI dysfunction, what do you do? There are various ways to address it.
- The first and most commonly used approach is to use specific enzymes which will break apart the biofilm. For example, proteolytic enzymes and polysaccharide-specific enzymes have been clinically proven to disrupt biofilm.
- Certain nutrients, such as N-Acetyl Cysteine (NAC), a precursor to the potent antioxidant glutathione, and monolaurin, which is an antimicrobial compound found in coconut oil, have also been shown to be effective in both disrupting biofilm and preventing the build up of new biofilm.
- Lastly, some herbal agents have the ability to interfere with quorum sensing, which is the way the microorganisms communicate with each other within the biofilm, and thus can be highly effective at breaking apart that biofilm.
It’s important to note that because of the incredible potency of biofilm disruption, it is recommended that you titrate up slowly over a period of a month to minimize detox reactions. As the biofilm are broken down, there will be die-off. Certain supports – such as monolaurin – work more gently and don’t need to be titrated.
How can you support your clients in this area?
Helping clients restore balance and resolve health issues is complex. There are so many layers involved – including something as small, yet significant as biofilm – that need to be effectively assessed and addressed in order to promote true, long-term healing. That is why we teach all things biofilm and more in our foundational class, Mastering the Art & Science of Gastrointestinal Healing. Because, it’s not until you have the tools to test for and truly understand what is going on within a client’s body will you have the information and insight to develop a custom protocol to help them finally heal.
If you’re ready to help your clients break through their healing barriers – including biofilm – check out Mastering the Art & Science of Gastrointestinal Healing. Our next class starts Tuesday, March 7th – but, hurry as seats are filling up!